The U.S. polio epidemic of the 1950s: A dreaded virus is finally controlled
Polio had been an endemic disease in the U.S. for many years before some would say it became a health crisis in the 1950s. “Sporadic cases of paralytic poliomyelitis have occurred for at least as long as human history,” wrote Dr. Joseph L. Melnick in his 1996 landmark article in the journal of the American Society for Microbiology.
Not a pandemic
Polio never reached the level of a pandemic. Epidemiologists are very careful about the use of that word, which indicates simultaneous world-wide epidemics.
However, the deaths and incurable consequences of paralysis from polio caused fear throughout the U.S. It left its mark on nearly every U.S. community including many in Wyoming. As an endemic virus, it was in the environment, causing one of those rare diseases that doctors were on the lookout for but couldn’t prevent.
That was true in other continents besides North America; the polio virus was in the background. Arctic-dwelling people were reported to develop cases equally in all age groups. In other locations it tended to affect infants and young children, especially in late summer months, Dr. Melnick reported.
Epidemics occurred
Occasionally it burst into epidemic levels in certain communities. A large outbreak occurred in New York City in 1916. In all of the U.S. that year, there were 27,000 cases and more than 6,000 deaths—one third of the deaths were in New York City alone, The borough of Brooklyn was the epicenter, where it affected mainly children under the age of five, according to Dr. Melnick.
An epidemiologist, Dr. Melnick (1914-2001) has been hailed as a founder of modern virology. The New York Times reported in his obituary that he and his associates also discovered how polio spreads. As people suspected, it was through water contaminated with the virus in fecal material. People with the virus did not always show symptoms but could excrete the virus. Occasionally flies were shown to transmit the virus, too.
“Infantile paralysis”
For a while, the disease had another name: “infantile paralysis.” Most cases were in children, but when it affected adults, it was often called “bulbar poliomyelitis,” implying that was a separate disease. In fact the virus is the same, but ”bulbar” meant the nerves of the mouth area were affected, making it difficult for the patient to breathe or swallow.
It didn’t seem right to say an adult came down with an “infantile” disease, so the bulbar term was used—sometimes inaccurately—regardless of which nerves were affected.
Franklin Delano Roosevelt came down with the disease in 1921, twelve years before he became president. In 1938 he founded the National Foundation for Infantile Paralysis. That year a comedian, Eddie Cantor, suggested that people send dimes to Roosevelt, to fund research. Thus the “March of Dimes” began and, in 1946, FDR’s profile was placed on the U.S. dime.
Today, a backward look at FDR’s symptoms point to a disease other than polio. Instead, his paralysis was most likely caused by a very rare autoimmune disorder discovered in 1916 and called Guillain-Barré, a non-viral disease. Years later a spinal tap also called lumbar puncture would have revealed whether or not there was a viral infection. But in 1921 it was only a highly controversial treatment in which spinal fluid was withdrawn or substances like diphtheria antitoxin were injected. It was not a diagnostic tool. Those “treatments” were ineffective and often fatal.
By at least 1947, a spinal tap was used to diagnose polio. In that year, Connie Howe Tyndall of Laramie recalls that she and her brother both had that procedure when they both were diagnosed, at age 13 and 2 respectively. They lived in Cody at the time and showed symptoms of muscular involvement for which they were hospitalized.
Worst U.S. epidemic—1952
In the U.S., there were 57,628 cases reported in 1952, with 3,145 deaths or a 5.7% death rate. This was truly alarming. Contaminated water was thought to be a source of the virus, and as a result swimming pools were shut down all over the country. Laramie didn’t have a municipal pool or a functioning one indoors at what is now the Civic Center (it was the high school in the 1950s), so that wasn’t an issue here.
Municipal water supplies were inspected; if done correctly, standard treatment killed viruses including the one causing polio. In Laramie this was happening at the same time that a local dentist, Dr. Charles Stebner, was urging that fluoride be added to the drinking water. City councilors were understandably reluctant to tinker with the water system then.
Cases continued throughout 1952 and through 1955. My sister-in-law, Nancy Knight Heintz, born in 1950, was infected with it during this period, in Clear Lake, SD. She recovered, but was afflicted with night-time seizures for a while afterward that her older brother (my husband) remembers. Medications for the seizures helped, and that effect which may or may not have been a symptom of polio gradually disappeared. Connie Tyndall reports that both she and her brother had leg aches that diminished as they got older and exercised more.
In Laramie, business as usual
A scan of local newspapers between 1952 and 1955 in the summer months when incidences were highest, shows mostly business as usual in Laramie.
On August 15, 1952, the Laramie Republican-Boomerang published an editorial titled “Fighting Polio” which had been written by a doctor for a syndicated news service. He suggested to anxious parents that children be given bed rest whenever they showed signs of illness until it was clear they didn’t have polio. At the time, physical activity was thought to make paralysis worse.
That wasn’t very helpful, because, as the doctor pointed out, in 1952 there still wasn’t an easy way to correctly diagnose polio early on. When symptoms of nervous system and muscular effects developed, the invasive spinal tap was used but wasn’t used for the common cold or flu.
However, it appears that the disease was not as widespread in Wyoming as elsewhere. In September of 1952 the newspaper reported a total of 48 cases of polio statewide. That compared to 58 cases the year before at the same time. The report was not broken down by counties.
Adults affected
However, it was front-page news when adults came down with polio. In 1953 there were three cases reported in the Laramie Bulletin newspaper. One was Dr. Frank R. Crocker, an optometrist in Rock Springs. He was flown to Salt Lake City by the Air Force at the request of the National Foundation for Infantile Paralysis. On September 11, 1953, two housewives in Rawlins came down with polio and were transferred to the hospital in Casper.
There were no mentions of childhood cases in the Laramie papers that I could find. However, Laramie native Peter Lindahl recalls that there were two adults in Laramie who developed polio, John Hamilton (1910-1990) and Paul Hall. Both worked in the UW College of Agriculture.
Lindahl remembers going with his parents to visit Hamilton in an iron lung in the hospital in Cheyenne. He recovered and was able to continue his work as an agricultural chemist at UW, though he suffered partial leg paralysis. He lived to be 80 and tolerated leg braces and crutches for the rest of his life. Paul Hall was a seed scientist at UW and died in 2000 at the age of 82. Lindahl recalls that he, too, used braces and crutches after having polio.
Certainly there must have been some Laramie children who were affected, but apparently most, like Connie Howe in Cody, managed to recover without paralysis. This was typical of most cases—it is thought now that only 1% of the cases developed severe paralysis.
Better sanitation a culprit?
But that other 99% could also pass the polio virus into the environment where it remained. An article on Next Nature Network, an Amsterdam-based futuristic technology alliance, theorizes that the increase in polio epidemics after 1900 was actually an unintended consequence of modern sewage treatment.
Its reasoning, echoed by others, is that pre-1900 everyone ingested some of the virus from water and most mothers developed antibodies to fight it, then passed their immunity on to their babies. Those babies matured and when the maternal immunity wore off, developed their own antibodies. But the cycle was broken when mothers didn’t develop antibodies because the water had no virus in it anymore, thus the babies were especially vulnerable.
Vaccine at last!
Many laboratories across the country were scrambling to develop a vaccine for polio. One became widely available in late August 1955. That is when Laramie received its first shipment, which came from Wyeth Laboratories in Pennsylvania. The state health department had decided that the first doses would be distributed to private physicians’ offices proportionately by population, and would be reserved for children between ages five and nine, apparently the most affected in Wyoming.
This first vaccine in Laramie was the one developed by Dr. Jonas Salk, who became a national hero for the work he did to develop it. The virus in it is rendered “dead” which makes it less potent than the type that came later. Two doses were necessary. Germaine St. John remembers the sugar cube with the red stain in the middle that was the first of two doses that she would have gotten in Laramie in 1955.
I got the same version in New Jersey while I was in high school, and remember being wary of the red dot that looked so much like blood. But I didn’t give it more than a momentary hesitation before swallowing the sugar cube. My parents were like Connie Howe Tyndall, then a Laramie resident, young mother and polio survivor, in making sure that their children got the vaccine.
Recent advances in polio vaccines include a live virus version, the Sabin vaccine. It now has additives that make it unnecessary to refrigerate as well as other changes that make it effective for mass innoculations in developing countries.
Polio today
Imagine the problem of vaccinating children in war-torn Syria today. Some children there were infected with a strain of the live virus that had been given to other children. The ones who had been vaccinated were protected; the ones who had been missed were highly susceptible to a mutation of the virus that the other children had received. That was reported in 2017, but within a year the World Health Organization (WHO) was on top of that outbreak, despite the complexity of finding the children and treating them.
There are three different strains of “wild” polio virus in the environment, all causing the same symptoms. Two have been eradicated since 2015. There is only one strain left, in Afghanistan and Pakistan. As reported by VOX news there were 94 cases in 2019, all in those two countries. The political climate there makes for more than the usual obstacles for health workers for whom eradication of polio is a high priority.
But this is a big change from the 350,000 cases of polio in 125 countries that the WHO reported in 1988. That is the year when the WHO (a United Nations agency based in Geneva, Switzerland) began its goal of eradicating polio. Now, in March of 2020, Switzerland itself is under strict quarantine as another virus makes its way through Europe and the rest of the world in what is now called a true pandemic.
By Judy Knight
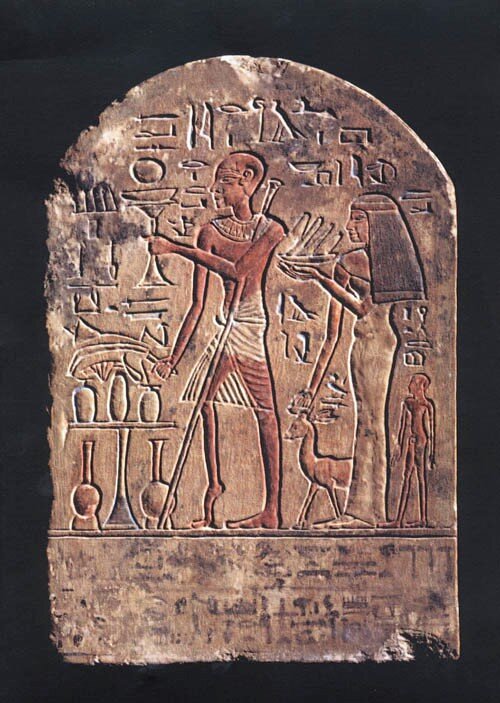
Source: photo by German photographer Fixi, as published in Wikipedia under Creative Commons license.
Caption: A Egyptian Stele (funerary) carving, apparently showing a polio victim with characteristic crutch and withered leg, from 1403-1365 BC.